CIO.com's senior editor covering healthcare IT looks back at what he thought was going to happen in 2013.
For those who follow healthcare IT — heck, even for those who don’t — 2013 will be remembered as The Year of Healthcare.gov. The failings of the federal health insurance marketplace dominated headlines. What’s more, the site’s troubles surprised many people but, admittedly, not everyone.
In January, I offered 13 predictions for 2013, which I expected to be a very active, not to mention interesting, year for healthcare information technology. It was indeed both active and interesting — just not always as I’d thought. Here’s a look back at what I thought would happen — and whether I was right or wrong.
Meaningful Use

Prediction: The ONC will give meaningful use a long, hard look. Was I right? Yes. (Off to a good start.)
As the year began, many had deemed Stage 2 of meaningful use, with its emphases on health information exchange and patient engagement, too complex for providers, who already have numerous technology and government quality reporting initiatives on their collective plates, as well as EHR vendors, who struggled with the rigors of updating their software and getting it certified.
So on Dec. 6, CMS announced another one-year extension of meaningful use. It’s admittedly a mixed bag: Yes, Stage 3 won’t start until 2017, but stage 2 still begins in 2014 for anyone who attested to stage 1 in 2011 or 2012.
Personal Health

Prediction: Personal health will finally catch on. Was I right? Not really.
I want personal health to catch on. The more the quantified self movement catches on, the more people know about their health and the more people are able to make informed decisions about not just healthcare but diet, exercise and overall wellness. This reduces healthcare costs for everyone, since healthy people go to the doctor less than sick people.
However, until wellness apps effectively connect patients to their physicians, and unless mobile health can fix its glaring yet largely ignored security problems, personal health will largely remain the purview of early adopters and the worried well.
Telemedicine

Prediction: Telemedicine will spread its wings. Was I right? Mostly.
Telemedicine tends to be an easy win for healthcare organizations, especially as videoconferencing and collaboration technologies advance and, increasingly, go mobile. It helps smaller, often rural providers offer better care by, say, connecting to university hospital systems for after-hours stroke treatment, and it gives those larger systems an additional revenue opportunity. It lets pharmacies and retailers get into the business of providing care — and address the long wait times for appointments that drive so many patients to the emergency room — by virtually connecting patients with doctors. Finally, it eases the transition from hospital to home with remote patient monitoring tools.
Health Information Exchange
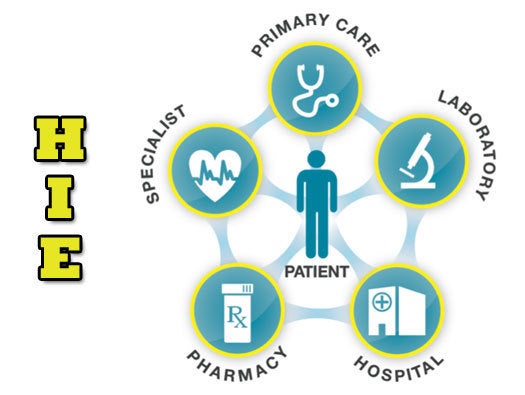
Prediction: The success of health information exchange will spread. Was I right? Mostly.
The United States still doesn’t have a national HIE entity, and no HIE standards have been set in clay, let alone stone, but 2013 did see many localized “wins” for health information exchange. Initiatives are advancing in many states, hitherto competing organizations are sharing data, and patients records are crossing state lines and even oceans. On top of that, the CommonWell Alliance, announced at HIMSS13, has started its first interoperability pilot, which will help the industry address what’s arguably the biggest barrier to health information exchange. (Well, that and paper.)
Accountable Care Organizations
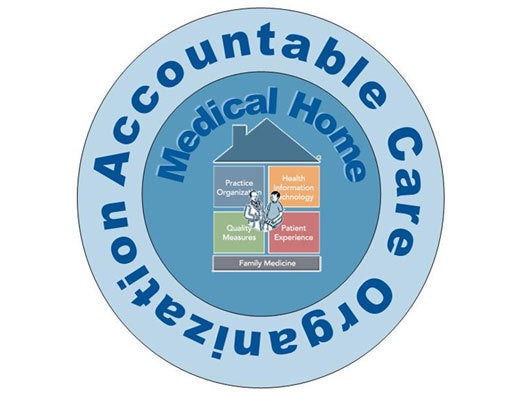
Prediction: Accountable care organizations will mature. Was I right? Not really.
The ACO model is often touted as the embodiment of healthcare reform: An integrated system that eschews the fee-for-service model to focus on shared savings through better care coordination. Unfortunately, it’s easier said than done. This summer, nine hospitals left the Pioneer ACO program, out of 32 participants, and only 13 produced “shared savings” that went back to the government. One critic suggests that the (flawed) ACO model aims to be “one big thing” rather than a “dozen smaller things” that, collectively, could better cut Medicare costs. It certainly doesn’t help that ACOs face daunting IT challenges, not to mention a strict 2016 deadline for demonstrating savings.
How’d I Do?

Image by bahri altay
Even taking into account my attempts to be vague and general — Security will be important? Gee, ya think? — I was sort of right eight times and kind of wrong five times. (I’d like to think my mediocrity stems from being so forward-thinking that I predicted certain trends before they would happen, not from throwing proverbial darts at a metaphorical dartboard. Let’s go with that.)
Here’s hoping I do better with my 2014 predictions for healthcare IT — coming soon.